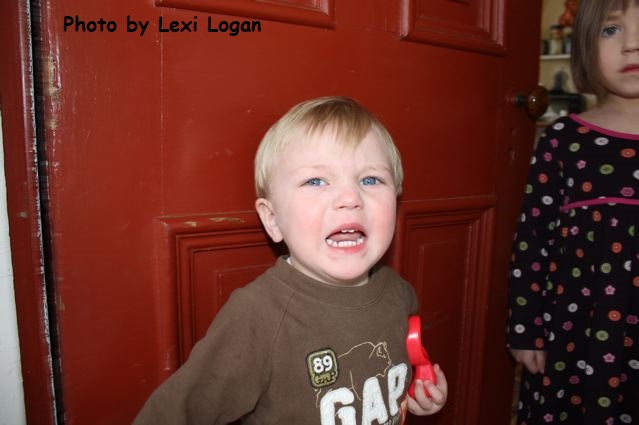
 Has your toddler ever pulled off your glasses and thrown them? Slapped another toddler at the playground? Bitten their brother? Run off in a store and ignored you when you called? Are you afraid to set limits for your child because you fear the tantrum that may result?
Has your toddler ever pulled off your glasses and thrown them? Slapped another toddler at the playground? Bitten their brother? Run off in a store and ignored you when you called? Are you afraid to set limits for your child because you fear the tantrum that may result?
Yes, toddlers are cute, but left to their own devices, they grow into the school bully, the family bully, or worse yet, they don’t listen to an adult and run into the street in front of a car.
Unbeknownst to you, you probably started to set limits for your child as early as 6 months of age.
If you breastfed, you may remember this scenario: you were breastfeeding your 6-month-old when they suddenly bit you very hard with their new tooth.
Did you continue to breastfeed calmly and ignore the mind numbing agony? Did you say in a sweet sing-song voice, “Honey, biting hurts Mommy. Mommy does not like being hurt. Please do not do that again?”
If you are like Dr. Kardos and Dr. Lai, you did not have time to say any of the above, because you were suddenly in PAIN. You likely removed your baby from your breast immediately and yelled, “OW!” Your baby (like each of ours) may have cried (howled) from surprise. However, your baby probably never bit you again while breast feeding!
Fast forward to the present and imagine you are holding your 16 month old and they hit, bite, pinch, pull your hair, or pull off your glasses. Maybe they were angry, but equally possible they may have been simply excited. Even though you know they are not purposefully hurting you, it is important to stop this behavior. Say in a firm voice: “No hitting!” and put them down.
This is time-out.
Time-out does not have to be spent on a chair in the corner of the room. Time-out is not a terrible punishment. Just like in sports, it is a pause in the play. By giving a time-out, your child learns that they do not get more attention for mean or aggressive behaviors, but less attention. As a variation, you can time-out a toy.
What if your baby starts crying on the floor? Give them a minute to recover. Remember that time-out lasts one minute per year of age. For your 16 month old, time-out will last one minute. At two years, time out will last two minutes. When time-out is complete, offer comfort. If they repeat the behavior, put them back down again.
Your goal, when you set limits for your child, is to stop a behavior that can hurt them or hurt others.
More tips on how to set limits:
Praise them specifically at every opportunity.
For example, “Good job putting your toys back into the box,” or “I like how you remembered to take my hand when we cross the street,” or “I like how you sit in your chair at dinner instead of standing up.” You will be amazed at how often children repeat desired behaviors that you point out to them.
Follow through on your requests.
If your toddler got a hold of a pair of scissors, you would take those scissors away immediately, without thought or fear about their feelings. You would put your child’s immediate safety ahead of their desire to play with scissors, and you would not stop to explain why they should give up this new-found plaything. Likewise, if you tell your child to come to you for any reason, be ready to physically go and lead them if they choose to ignore you. For instance, at a party, wait to tell them to come until you are ready to go. Otherwise they will learn that you “cry wolf” and will ignore you.
Make consequences logical and immediate for undesirable behaviors.
If your child throws a toy train at his friend’s house, say “No throwing trains!” and take the train away for a time-out. Telling them that “you are in trouble when we get home” means nothing to a toddler.
Refrain from explaining too much.
Toddlers have a TINY attention span. Just give them a command or an explanation that is 3-4 words or less. For example, “No hitting, it hurts!” is enough. Telling them that hitting hurts others, asking how would they like to be hit and telling them about the need to be kind, is wasted effort. The time for longer explanations is when they are developmentally capable of putting themselves in another’s shoes, around age six years for most children.
Label the behavior as bad, not the child.
Say “No throwing sand!” not “You are bad for throwing sand!”
Remember to set expectations and teach which behaviors are not acceptable.
Toddlers are not mind-readers. You need to tell them not to open the trash can and rummage through it, otherwise they will not know any better.
Seize the opportunity to turn a negative behavior into a positive behavior.
For instance, as you see your child raise their hand to hit you, firmly hold their wrist and say “Don’t hit. Soft touches,” and simultaneously bring their hand to pat your cheek. This will give you a chance to praise your child.
Do not fear the tantrum.
Toddler tantrums are NORMAL reactions to feeling angry or frustrated. Many toddlers throw tantrums in response to your telling them “no” or “stop.” It is not fair to expect toddlers not to throw tantrums. Just put on your bored face (and some ear plugs) and wait for it to be over.
If a tantrum immediately occurs, remind yourself that at least you stopped your child from hurting themselves or others. Tantrums don’t hurt anyone. You can read more about how to manage tantrums here.
Set limits for your child.
When you set limits for your child, you teach them to behave in ways that will keep them and others safe. Act confidently when you set limits, and your child will learn to interact appropriately with others and gain self-control.
Julie Kardos, MD and Naline Lai, MD
©2019 Two Peds in a Pod®





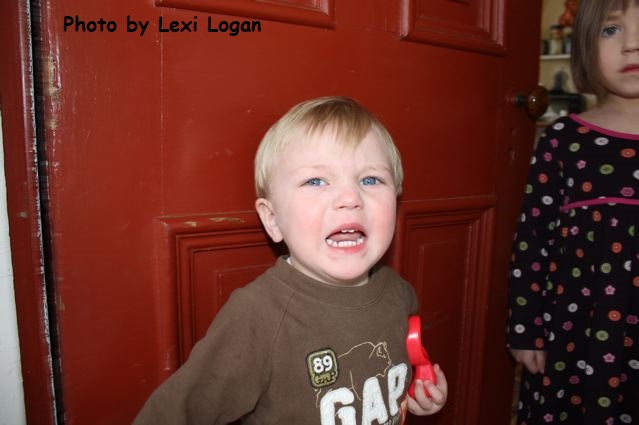 Has your toddler ever pulled off your glasses and thrown them? Slapped another toddler at the playground? Bitten their brother? Run off in a store and ignored you when you called?
Has your toddler ever pulled off your glasses and thrown them? Slapped another toddler at the playground? Bitten their brother? Run off in a store and ignored you when you called?  It’s pretty annoying to be itchy. Dr. Lai fondly called her itchy oldest child with eczema “itchy, bitty, spider,”or some variant of that, for much of her daughter’s childhood. Fortunately, for your kids with sensitive skin, dermatologist
It’s pretty annoying to be itchy. Dr. Lai fondly called her itchy oldest child with eczema “itchy, bitty, spider,”or some variant of that, for much of her daughter’s childhood. Fortunately, for your kids with sensitive skin, dermatologist  The type of moisturizer you select is very important. It is best to use an ointment (like plain unscented Vaseline™ or Aquaphor™) or a heavy cream (like Vanicream™, CeraVe™ cream, Cetaphil™ cream, or Aveeno™ Baby Eczema Therapy Moisturizing cream, to name a few). Lotions are poor choices because they tend to contain more preservatives and ingredients that can sting open skin or cause irritation.
The type of moisturizer you select is very important. It is best to use an ointment (like plain unscented Vaseline™ or Aquaphor™) or a heavy cream (like Vanicream™, CeraVe™ cream, Cetaphil™ cream, or Aveeno™ Baby Eczema Therapy Moisturizing cream, to name a few). Lotions are poor choices because they tend to contain more preservatives and ingredients that can sting open skin or cause irritation. Apply moisturizer to the skin at least twice daily, but more often if the child’s skin is unusually dry or the eczema is severe. Apply topical medications sparingly to the affected areas prior to the application of moisturizer. I recommend applying topical medications twice daily, but you should follow the instructions given by your child’s doctor. It is very important that medications are applied only to areas of active eczema and never to normal skin. Apply moisturizer to all skin, including over the areas where you already applied medication.
Apply moisturizer to the skin at least twice daily, but more often if the child’s skin is unusually dry or the eczema is severe. Apply topical medications sparingly to the affected areas prior to the application of moisturizer. I recommend applying topical medications twice daily, but you should follow the instructions given by your child’s doctor. It is very important that medications are applied only to areas of active eczema and never to normal skin. Apply moisturizer to all skin, including over the areas where you already applied medication.