A developmental guide to reading to your young child
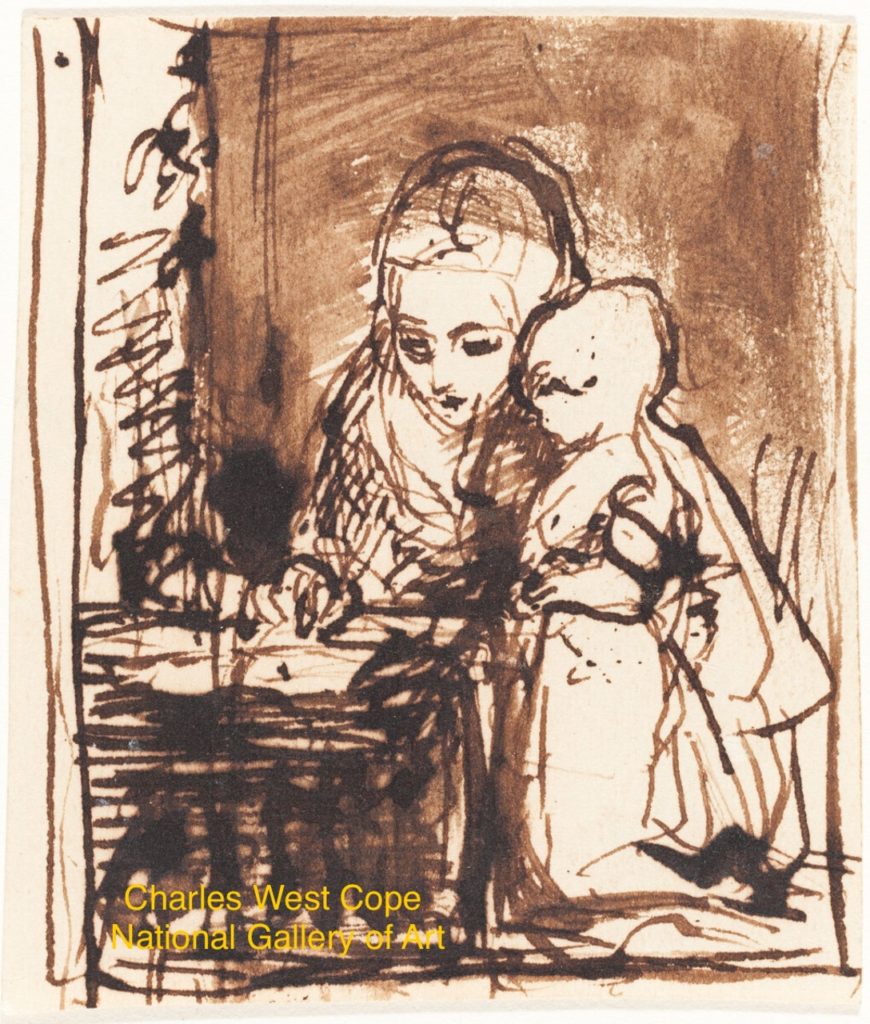
We know parents who started reading to their children before they were born, but don’t fret if you didn’t start when baby was in the womb. It’s never too late to start. Today we give you a developmental guide to reading with your young child.
Three months of age
By three months of age, most babies are sleeping more hours overnight and fewer hours during the day (and, hence, so are their parents). Now you have time to incorporate reading into your baby’s daily schedule. At this age babies can visually scan pictures on both pages of a book. Babies see better close-up, so you can either prop your baby on your lap with a book in front of both of you, or you can lie down next to your baby on the rug and hold the book up in front of both of you. The classic Goodnight, Moon by Margaret Wise Brown or any basic picture book is a great choice at this age.
Six months of age
By six months of age many babies sit alone or propped and it is easier to have a baby and book in your lap more comfortably. Board books work well at this age because 6-month-olds explore their environment by touching, looking, and MOUTHING. Sandra Boynton’s Moo, Baa, La La La was a favorite of Dr. Kardos’s twins at this age, both to read and to chew on.
Nine months of age
By nine months many babies get excited as you come to the same page of a known book that you always clap or laugh or make a funny noise or facial expression. They also enjoy books that involve touch, such as Pat the Bunny, by Dorothy Kunhardt.
One year
At one year, kids are often on the move. They learn even when they seem like they are not paying attention. At this age, your child may still want to sit in your lap for a book, or they may walk or cruise around the room while you read. One-year-olds may hand you a book for you to read to them. Don’t read just straight through a book, but point repeatedly at a picture and name it.
18 months old
By 18 months, kids can sit and turn pages of a book on their own. Flap books become entertaining for them because they have the fine motor skills that enable them to lift the flap. The age of “hunter/gatherer,” your 18-month-old may enjoy taking the books off of the shelf or out of a box or basket and then putting them back as much as they enjoy your reading the books.
Two-year-olds
Two-year-olds speak in two word sentences, so they can ask for “More book!” Kids this age enjoy rhyming and repetition books. Jamberry, by Bruce Degen, is one example. You can also point out pictures in a book and ask “What is that?” or “What is happening?” or “What is he doing?” Not only are you enjoying books together, but you are preparing your child for the culture of school, when teachers ask children questions that the teacher already knows the answers to.
Here is some magic you can work: you may be able to use books to halt an endless tantrum: take a book, sit across the room, and read in a soft, calm voice. Your child will need to quiet down in order to hear you and he may very well come crawling into your lap and saving face by listening to you read the book to him.
Three-year-olds
Three-year-olds ask “WHY?” and become interested in nonfiction books. They may enjoy a simple book about outer space, trucks, dinosaurs, sports, puppies, or weather. They can be stubborn at this age. Just as they may demand the same dinner night after night (oh no, not another plate of grilled cheese and strawberries!), they may demand the same exact book every single night at bedtime for weeks on end! Try introducing new books at other times of day when they may feel more adventurous, and indulge them in their favorite bedtime books for as long as they want. They may even memorize the book as they “read” the book themselves, even turning the pages at the correct time.
Four and five-year-olds
Four and five-year-olds have longer attention spans and may be ready for simple chapter books. For example, try the Henry and Mudge books by Cynthia Rylant. Kids this age still enjoy rhyming books (cue in Dr. Seuss) and simple story books. At four, kids remember parts of stories, so talk about a book outside of bedtime.
Some children this age know their letters and even have some sight words, but refrain from forcing your child to learn to read at this age. Studies show that by second grade, kids who have been exposed to books and reading in their homes are better readers than kids who have not, but the age children start to read does not correlate with later reading skills. So just enjoy books together.
E-readers and iPads
What about e-readers and books on ipads? The shared attention between a parent and a child is important for developing social and language skills, so share that ebook together.
Now that you have read our post, go read to your child, no matter how old he is. Even a ten-year-old enjoys sharing a book with their parents. Eventually, you will find your whole family reading the same book (although maybe at different times) and before you know it, you’ll have a book club…how nice, to have a book club and not worry about cleaning the house ahead of time…
Julie Kardos, MD and Naline Lai, MD
©2025 Two Peds in a Pod® originally posted in 2017